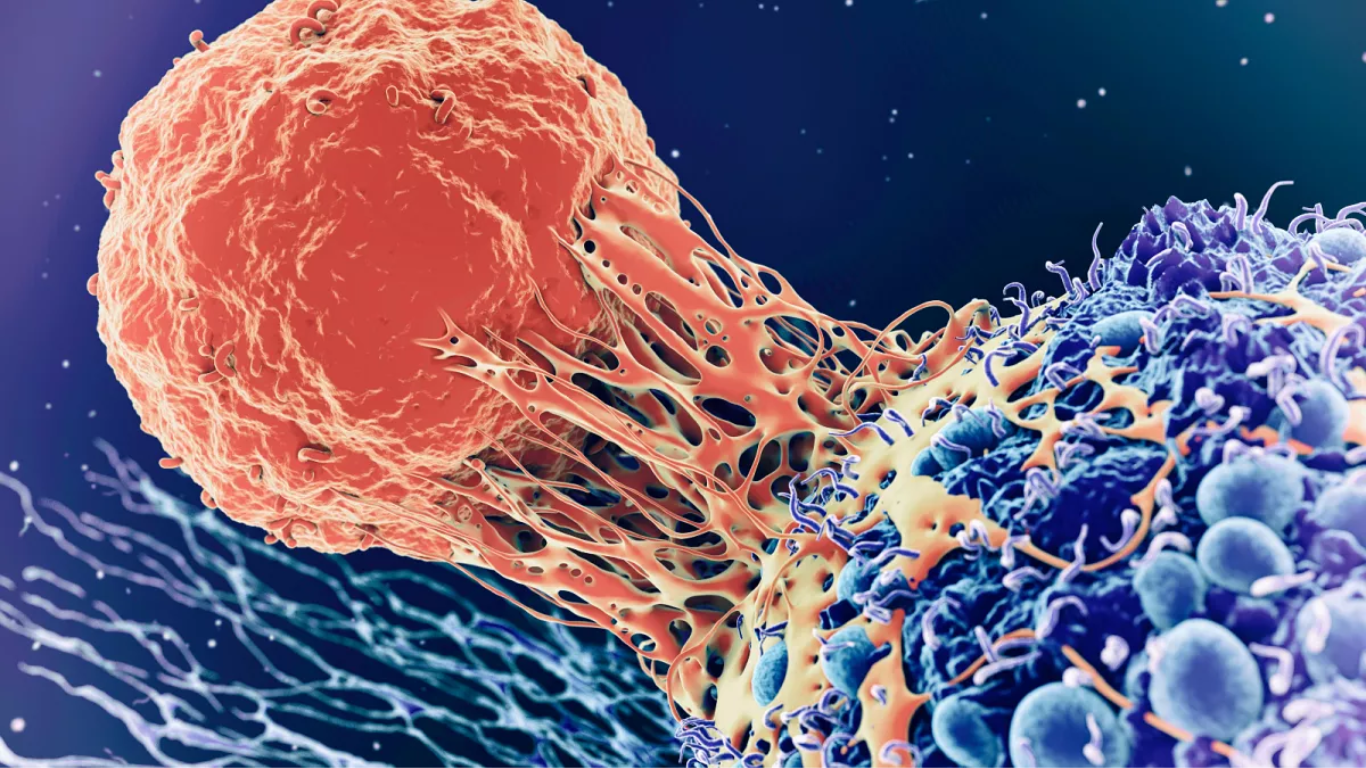



Many factors, including the sort of bacteria that ordinarily occupy the reproductive canal, may impact IVF conception rates. Probiotics with “good” bacteria are becoming increasingly popular in the treatment of vaginal microbiota disorders in women.
Probiotics, however, do not alter detrimental vaginal flora when administered to patients vaginally in the form of a daily pill for 10 days before to reproductive treatment, according to a recent research from The ReproHealth Research Consortium Zealand University Hospital. There was no statistically significant difference between these women and the placebo group.
However, regardless of whether they took a probiotic or not, more than a third (34%) of all women who participated in the experiment improved between a month and three months later.
On this premise, the authors propose that patients with a ‘unfavourable’ vaginal microbiome postpone reproductive therapy until a normal balance is attained.
The findings will be presented today at the 38th Annual Meeting of ESHRE by principal scientist Ida Engberg Jepsen from The Fertility Clinic at Zealand University Hospital in Denmark. She believes that the’spontaneous’ improvement rate reported among patients may warrant a shift in approach to IVF scheduling.
‘The study suggests that administering vaginal lactobacilli probiotics may not improve a suboptimal vaginal microbiome,’ she added.
‘However, a one-to-three-month spontaneous improvement rate may offer the basis for an alternate treatment strategy.’ The strategy would involve postponing fertility treatment until spontaneous improvement occurs, but further research is needed. The specific vaginal probiotic tested in this study had no effect on the favourability of the vaginal microbiome before IVF. But probiotics, in general, should not yet be discounted.’
Research has shown that pregnancy and live birth rates are higher among women whose vaginal microbiota is dominated by lactobacillus, a genus of lactic-acid-producing bacteria. Conversely, those with an imbalance – or dysbiosis – where the lactobacillus concentration is too low may have a lesser chance of an embryo implanting in the uterus.
The study was carried out at a university fertility clinic between April 2019 and February 2021. A total of 74 women referred for IVF treatment were recruited. All had an abnormal lactobacillus profile which varied from low to medium quality.
The women were randomly assigned either to receive vaginal probiotic capsules (n=38) or a placebo (n=36). Samples were taken to determine the effect on the vaginal microbiome following the 10-day course of probiotics, and again in the subsequent menstrual cycle (on cycle day 21 to 25). Improvement in the vaginal microbiome was defined as a shift in receptivity profile from low to medium; low to high; and from medium to high.
The vaginal microbiota improved by 40% in the placebo group and by 29% in the lactobacillus probiotic group, according to the findings. This was not a statistically significant difference. Following the intervention, similar results in the menstrual cycle were seen.
According to the authors, the probiotic samples included just two strains of lactobacilli. Furthermore, they claim that the wide classification of the vaginal microbiota profile may miss’more subtle alterations’ that might impair fertility.