AI Chatbot Exposes Hospital Fraud: Family Cuts ₹1.7 Crore Bill to ₹30 Lakh (Pc: X)
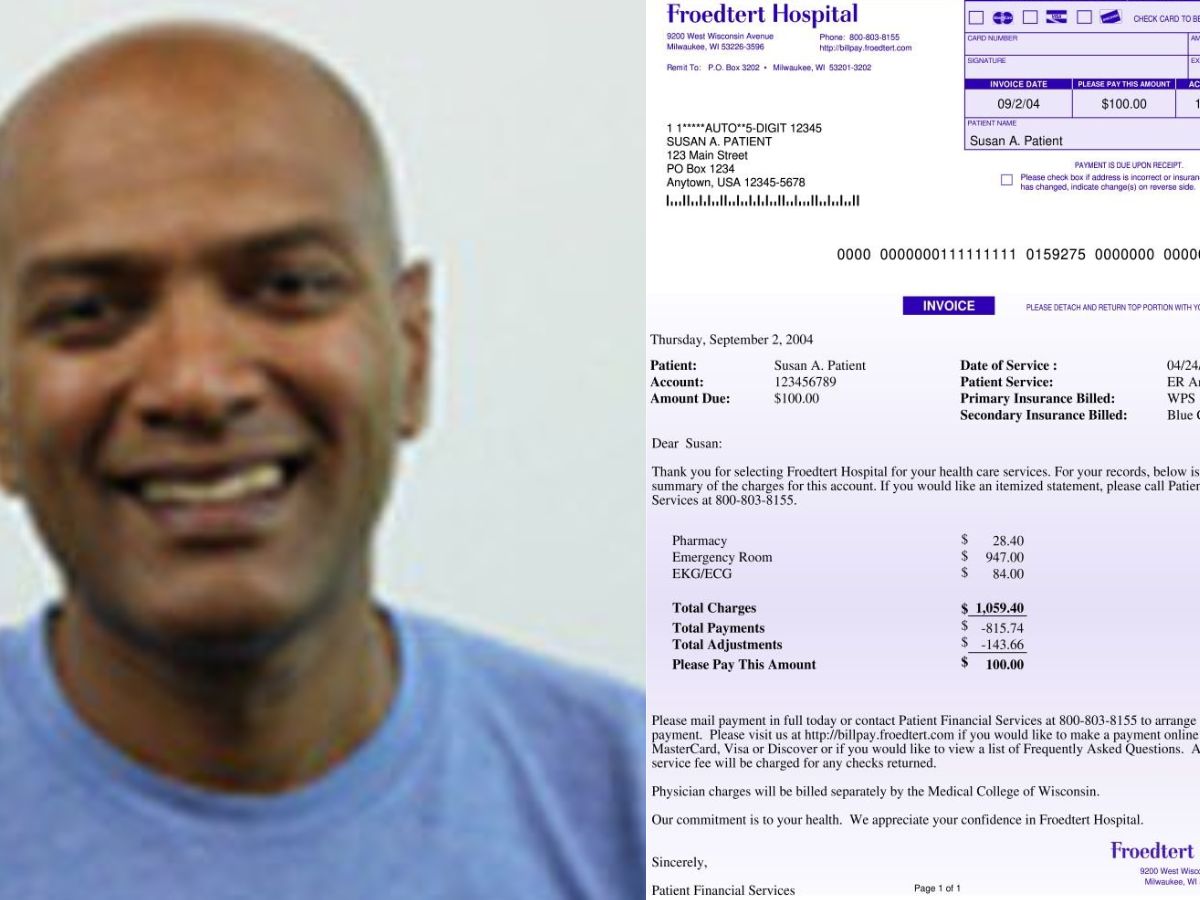
About a grieving family in the USA that formerly faced a $195,000 (or about ₹1.7 Crore) hospital bill after the death of a relative, for which they managed to bring the charge down to just $33,000 (or about ₹30 Lakh) using an AI chatbot called Claude.
The patient had barely been in intensive care for four hours, and the family had to battle with the entire opaque charge since his insurance had just lapsed. Instead of surrendering, one family member decided to input the bill and the complex CPT codes into the AI.
The results were astonishing: Claude expertly dissected the charges and discovered large billing mistakes that would never be seen by the naked eye. There were also approximately $100,000 in double charges; the hospital was billing the master procedure and then billing separately for every single component part a practice that is expressly prohibited by common regulatory standards, like Medicare.
The family used this forensic review to draft assertive, legal-sounding letters demanding a fair price, which, in the end, forced the hospital to bend to their will.
The family has been very successful: a serious question now: Did the hospital commit fraud? The mere identification of matters this widespread and systematic like double billing for procedures tends dangerously toward the realm of deception or outright fraud.
The hospital negotiating down to an unbelievably low sum very quickly would seem to indicate acknowledgement that their original bill could not withstand scrutiny in court or public opinion.
While, of course, criminal intent could be substantiated through official regulatory investigations, this case does starkly illustrate the obvious: that medical billing is an arena often hidden behind complex systems deliberately engineered to deceive financially naive patients.
The chatbot, in this case, acted like a most powerful tireless consumer advocacy agency that effectively balanced the thorough information of an individual and massive healthcare institution.
Herein lies a blaring wake-up call for regulators and oversight bodies to review their modus operandi: the fact that a commercially available AI tool could uncover what amounted to a $162,000 overcharge in almost no time demonstrates that these issues with medical bill fraud are probably quite widespread and systematic, and not just singular, isolated “human errors.”
AI as an entity is now capable of auditing, challenging, and negotiating, thereby empowering consumers to rise against a system that had, for far too long, counted on patient ignorance. It is this technology that has created for the first time an unprecedented demand for transparency, which essentially presses healthcare providers to either reform their charging practices or be prepared to face the public and legal wrath for their sheer opacity.
A recent media graduate, Bhumi Vashisht is currently making a significant contribution as a committed content writer. She brings new ideas to the media sector and is an expert at creating strategic content and captivating tales, having working in the field from past four months.
Virat Kohli’s Instagram account disappears, leaving fans puzzled. Many flood Anushka Sharma’s page asking, “Bhaabhi,…
Dhurandhar OTT Release: Ranveer Singh’s ₹1300 Cr spy thriller premieres on Netflix Jan 30; set…
EU designates Iran’s IRGC as a terrorist organisation: Force reporting to Ali Khamenei sanctioned amid…